Radiation Dose Distribution of a Surgeon and Medical Staff during Orthopedic Balloon Kyphoplasty in Japan
Article information
Abstract
Background
The present study investigated the radiation dose distribution of balloon kyphoplasty (BKP) among surgeons and medical staff, and this is the first research to observe such exposure in Japan.
Materials and Methods
The study subjects were an orthopedic surgeon (n=1) and surgical staff (n=9) who intervened in BKP surgery performed at the National Hospital Organization Disaster Medical Center (Tokyo, Japan) between March 2019 and October 2019. Only disposable protective gloves (0.022 mmPb equivalent thickness or less) and trunk protectors were used, and no protective glasses or thyroid drapes were used.
Results and Discussion
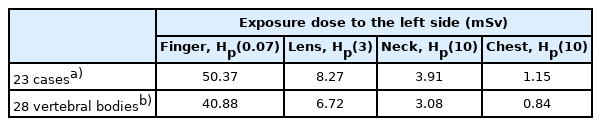
The surgery time per vertebral body was 36.2 minutes, and the fluoroscopic time was 6.8 minutes. The average exposure dose per vertebral body was 1.46 mSv for the finger (70 μm dose equivalent), 0.24 mSv for the lens of the eye (3 mm dose equivalent), 0.11 mSv for the neck (10 mm dose equivalent), and 0.03 mSv for the chest (10 mm dose equivalent) under the protective suit. The estimated cumulative radiation exposure dose of 23 cases of BKP was calculated to be 50.37 mSv for the fingers, 8.27 mSv for the lens, 3.91 mSv for the neck, and 1.15 mSv for the chest.
Conclusion
It is important to know the exposure dose of orthopedic surgeons, implement measures for exposure reduction, and verify the safety of daily use of radiation during surgery and examination.
Introduction
It has been reported that chronic radiation skin disorders among medical workers have been certified as an occupational injury in Japan [1]. In April 2011, the International Commission on Radiological Protection (ICRP) published a statement on tissue reactions, recommending an equivalent dose limit for the lens of the eye to be 20 mSv per annum [2]. The ICRP reported that recent epidemiological findings suggest threshold doses lower than previous knowledge for some of the tissue response effects, especially those that develop very late [3]. Based on this, the International Atomic Energy Agency (IAEA) has proposed that, for occupational exposures, the equivalent eye lens dose limit has been decreased to 20 mSv per year for a specified 5-year average and no more than 50 mSv in each 1 year from the current limit of 150 mSv per year [4]. Mastrangelo et al. [5] has reported that orthopedic surgeons have approximately 2–5 times higher cancer incidence compared to non-orthopedic surgeons, radiation-exposed non-doctors, and non-exposed workers. They suggested that many orthopedic surgeries are performed under X-ray fluoroscopy, and fluoroscopy has been widely used to identify fracture sites and evaluate medical procedures. Among them, balloon kyphoplasty (BKP), a new treatment for vertebral compression fractures [6–10], requires a relatively short surgery time but is performed under continuous fluoroscopy. Radiation exposure of surgeons, chiefly fingers that cannot be avoided in fluoroscopy, is expected to be at high doses. With the aging of the population, the number of cases of BKP treating spinal compression fractures due to osteoporosis, trauma, metastases, and myeloma is expected to increase. The radiation safety protection for surgeons cannot be updated without investigation of radiation exposure during BKP. The evaluations of BKP radiation exposure of patients have been conducted in Western countries [11–13]. BKP can be associated with significant radiation exposure to the operators [14]. However, few reports are available on the evaluation of BKP radiation exposure in Japan. To investigate the radiation dose distribution of BKP, we conducted descriptive research among an orthopedic surgeon and medical staff.
Materials and Methods
1. Study Subjects
The study subjects were an orthopedic surgeon (n=1) and surgical staff (n=9) who intervened in BKP surgery performed at the National Hospital Organization Disaster Medical Center (Tokyo, Japan) between March 2019 and October 2019. The surgical staff included assistant surgeons, scrub nurses, and circulating nurses. This study was approved by the Institutional Ethics Committee of the National Hospital Organization Disaster Medical Center and National Institute (Public Receipt No. NIPH-IBRA 12236) and Tokyo Healthcare University (Receipt No. 30-54). Written informed consent was obtained.
2. Measurements
We recorded the number of vertebral bodies per surgery, the surgery time (minutes), the fluoroscopic time (minutes), and the exposure dose of the staff involved in the surgery. The positions of the surgeon and the staff during surgery were as follows: the surgeon was on the left side of the patient in the prone position, the assisting physician was on the right side of the patient, and the scrub nurse was behind the surgeon (Fig. 1). The distance from the patient’s surface to the upper C-arm surfaces was approximately 30–35 cm (Fig. 2).

The positions of the surgeon and the staff during surgery: the surgeon on the left side of the patient in the prone position, the assisting physician on the right side of the patient in the main position, and the scrub nurse behind the surgeon.
Table 1 shows the types of dosimeters used and the measurement sites. The measurement sites for the surgeon were the left ring finger (70 μm dose equivalent) with disposable protective gloves (0.022 mmPb equivalent thickness or less), left eye lens (3 mm dose equivalent), and left neck/chest (10 mm dose equivalent). The glass ring dosimeter (JK type) for X- and γ rays was sterilized for each surgery by plasma sterilization recommended by the manufacturer. For the surgical assistants, we measured exposure at the left eye lens (3 mm dose equivalent) and the left neck/chest (10 mm dose equivalent). For nurses, exposure was measured on the left chest and abdomen for men and the left abdomen (10 mm dose equivalent) for women. Each measurement was recorded as a cumulative dose for two months. A glass ring dosimeter (JK type) for X- and γ rays for the left ring finger, DOSIRIS dosimeters (Chiyoda Technol Corp., Tokyo, Japan) for the eye lenses and glass badge X-ray dosimeters (FX type; Chiyoda Technol Corp.) for the next and chest were used, respectively. All staff wore protective clothing (0.35 mmPb equivalent thickness) on their trunks and personal real-time dose dosimeters (MyDose Mini X, Chiyoda Technol Corp.), under the protective clothing to determine the exposure dose for each surgery. For background measurements, spare glass dosimeters were prepared and measured. All the glass dosimeters were analyzed by the Chiyoda Technol Corp. Measurements were taken on the trunk (chest for men, abdomen for women). Two X-ray fluoroscopes (Fujifilm, Tokyo, Japan; Siemens, Munich, Germany) and a C-arm manufactured by Philips were used during surgery. The exposure parameters of the X-ray fluoroscope were determined by automatic brightness control.
Results and Discussion
A total of 10 cases (15 vertebral bodies) underwent BKP during the 8-month study period. The total surgery and fluoroscopy time was 544.0 and 109.4 minutes, while the average surgery and fluoroscopy time was 54.4 (min–max, 30–129 minutes) and 10.2 minutes (min-max, 4.1–31.4 minutes), respectively. The cumulative radiation chest exposure dose measured by the real-time dosimeters was 500 μSv for the surgeon under the protective suit, 3 μSv for the assisting physician on the left side under the protective suit, 291 μSv on the right side, and 0 μSv for the nurse under the protective suit (Table 2). Tables 3–6 show the exposure dose distribution by measurement site for the surgeon and medical staff. The cumulative radiation exposure dose of the surgeon was 21.9 mSv for the finger (70 μm dose equivalent), 3.6 mSv for the lens (3 mm dose equivalent), 1.7 mSv for the neck (10 mm dose equivalent), and 0.5 mSv for the chest (10 mm dose equivalent), respectively. The cumulative doses of the assisting physicians were below the detection limit for the crystalline lens (3 mm dose equivalent), 0.2 mSv for the neck (10 mm dose equivalent), and below the detection limit for the chest (10 mm dose equivalent). The cumulative doses of the nurses (including circulating nurses) were below the detection limit for the abdomen (10 mm dose equivalent). There was no measurement difference in the cumulative radiation doses between the real-time dosimeter and the glass dosimeter (FX model). The surgery time per vertebral body was 36.2 minutes, and the fluoroscopic time was 6.8 minutes. The average exposure dose per vertebral body was 1.46 mSv for the finger (70 μm dose equivalent), 0.24 mSv for the lens (3 mm dose equivalent), 0.11 mSv for the neck (10 mm dose equivalent), and 0.03 mSv for the chest (10 mm dose equivalent) under the protective suit, respectively. This shows that the exposure dose to the fingers is the highest, followed by the crystalline lens and the neck.
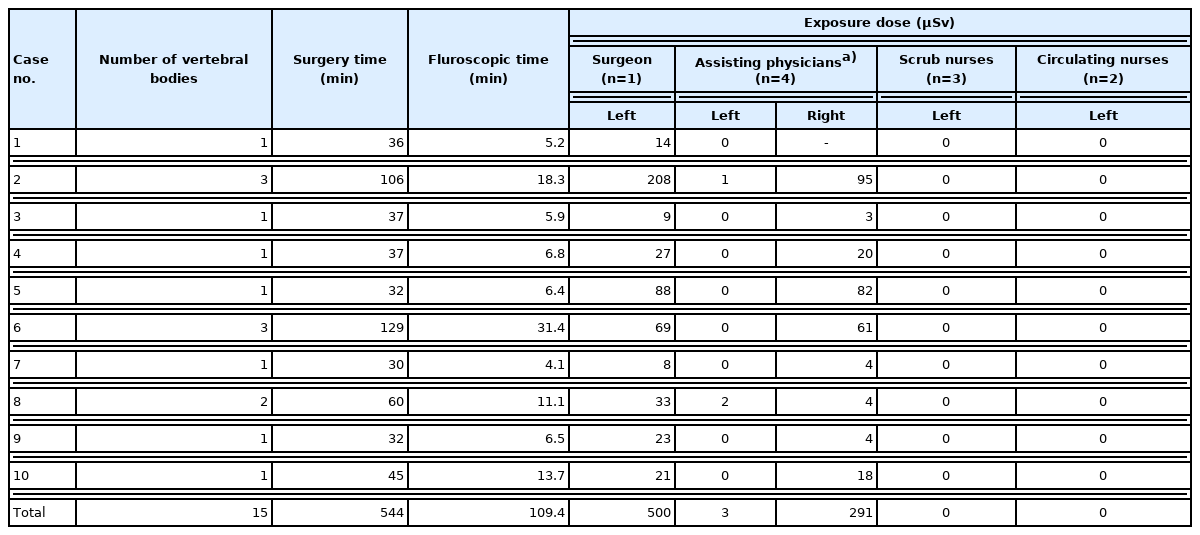
Chest (surgeon and assisting physicians) and abdomen (nurses) radiation exposure dose per case measured by real-time dosimeters (MyDose Mini X) under the protective suit
The number of orthopedic surgery cases by the surgeon in 2018 was 189 cases, of which 23 cases were BKP, involving 28 vertebral bodies, and total surgery time was 1,076 minutes. Based on the measurements taken during this study, the cumulative radiation exposure dose for 23 cases of BKP was estimated to be 50.37 mSv for the fingers, 8.27 mSv for the lens, 3.91 mSv for the neck, and 1.15 mSv for the chest, and the estimated dose for 28 vertebral bodies was calculated to be 40.88 mSv, 6.72 mSv, 3.08 mSv, and 0.84 mSv, respectively (Table 6). The surgeon and assisting physicians were wearing glasses for vision correction.
A previous study of hand exposure during fluoroscopy investigated a total of 97 fluoroscopy procedures over 14 months, with the operating time of 4,954 minutes, X-ray exposure time of 437 minutes. The exposure dose was 1.4 mSv in the cervix and 32.5 mSv in total direct exposure to the fingers (average 0.34 mSv per event) [15]. Under fluoroscopy in the field of orthopedics, the direct exposure to the fingers was reported to be 0.18 mSv and 0.2 mSv per case [16, 17]. In this study, the exposure dose to the operator’s fingers was 21.9 mSv (average of 2.19 mSv per event) in ten cases of BKP surgery. BKP surgery has been suggested to induce high radiation exposure to operator’s fingers. In 2018, the surgeon in this study performed 189 cases of orthopedic surgeries, of which 23 cases (28 vertebral bodies) were BKP with a total surgery time of 1,076 minutes. Based on the results of this study, the hand exposure dose in 23 cases of BKP was estimated to be 50.37 mSv. This does not reach the equivalent dose annual limit to the skin recommended by the ICRP of less than 500 mSv for clinicians who use radiations and does not cause tissue damage. However, there is a report that protective equipment was not properly used during surgery, and the low usage of disposable protective gloves during procedures and treatments involving fluoroscopy was common in Japan [18]. Exposure doses could have been higher without the use of disposable protective gloves. The actual exposure of the hands and fingers is expected to be even higher in the cases of fluoroscopic surgery, root block, and myelography.
The total dose to the surgeon’s crystalline lens during the ten cases of BKP in this study was 3.6 mSv. Based on the results of this study, the estimated dose of lens exposure for the surgeon during BKP surgeries in 2018 was 8.28 mSv. The ICRP recommends that the equivalent dose limit for the eye lens should not exceed 20 mSv per year over a 5-year period and 50 mSv in any 1 year, and our result was below the standard level [2]. However, the actual cumulative dose of the lens remains unknown because the radiation dose from other radiation-using procedures is unknown. The exposure dose to the lens and chest of the surgical assistants (physicians) was below the detection limit, and the equivalent dose to the neck was measured to be 0.2 mSv in two surgeries. A single measurement recorded by a personal exposure dosimeter was high (291 μSv) on the X-ray fluoroscope side. It suggests that the crystalline lens on the X-ray fluoroscopy device side is exposed to a higher dose, and it is necessary to measure the dose on the side in future studies. Since the nurse’s thoracoabdominal dosimeter measurements were below the detection limit, the protective gears can protect the wearers against scattered radiation when properly used. In the BKP conducted in this study, keeping a sufficient distance from the radiation source was difficult for the surgeon, and the use of the pulse fluoroscopy mode was effective when the fingers directly entered the X-ray irradiation field. Therefore, it is worth considering broader applications of pulse fluoroscopy with surgeons. Only disposable protective gloves (0.022 mmPb equivalent thickness or less) and trunk protectors were used, and no protective glasses or thyroid drapes were used. Several previous studies have shown that heavy workloads can reach the annual limit dose to the lens and sometimes exceed it, and recommend the use of protective glasses [19, 20]. Several reports indicate that the use of protective glasses with a 0.07 mmPb equivalent thickness have a radiation reduction effect of about 50%–60% under cardiovascular catheterization [21, 22]. It has been reported that the use of lead glass goggles with an equivalent thickness of 0.75 mmPb reduced the dose to the lens by 91.2% (at a distance of 0.6 m from the phantom) in spinal surgery [23]. Therefore, protective glasses are expected to have radiation protective effects in the BKP procedure. Synowitz and Kiwit [24] emphasized the importance of surgeons wearing lead glove protection on their leading hands during percutaneous vertebroplasty procedures and demonstrated a 75% reduction rate of exposure to radiation. Orthopedic surgeons and assisting physicians should consider wearing radiation protection glasses and glove, keeping their hands out of the radiation beam, and avoiding of unnecessary fluoroscopic images during BKP surgeries to reduce the exposure of the eye lenses.
Conclusion
It is important to know the exposure dose of orthopedic surgeons, implement proper measures to reduce exposure, and verify the safety of daily use of radiation by examining each surgery and examination.
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
Conceptualization: Ono K. Formal analysis: Kumasawa T. Funding acquisition: Kunugita N. Project administration: Yamaguchi C. Visualization: Kanou M. Writing - original draft: Ono K. Writing - review and editing: Ono K, Shimatani K. Approval of final manuscript: all authors.
Acknowledgements
This work was supported in part by the Industrial Disease Clinical Research, Japan. N. Kunugita was supported by Japanese Ministry of Health, Labour and Welfare (Grant No. 180501-1).
We thank Dr. H. Matsuzaki, Mr. S. Kagayama, and Mr. H. Yoshida in National Hospital Organization Disaster Medical Center for their coordination, supervision, and data collection. We also appreciate Ms. Ichika and the medical staff in National Hospital Organization Disaster Medical Center for their study support.